Gingivitis
Gingivitis (bleeding gums) is an infection caused by bacteria. In around 12 to 24 hours the natural bacteria in the mouth will reproduce and form a sticky, almost invisible, film on the teeth called plaque. If this plaque (bio-film) is not removed by brushing and an effective oral hygiene regime at home then it will develop into calculus (tartar). As the inflammation progresses, various signs and symptoms will begin to become obvious.
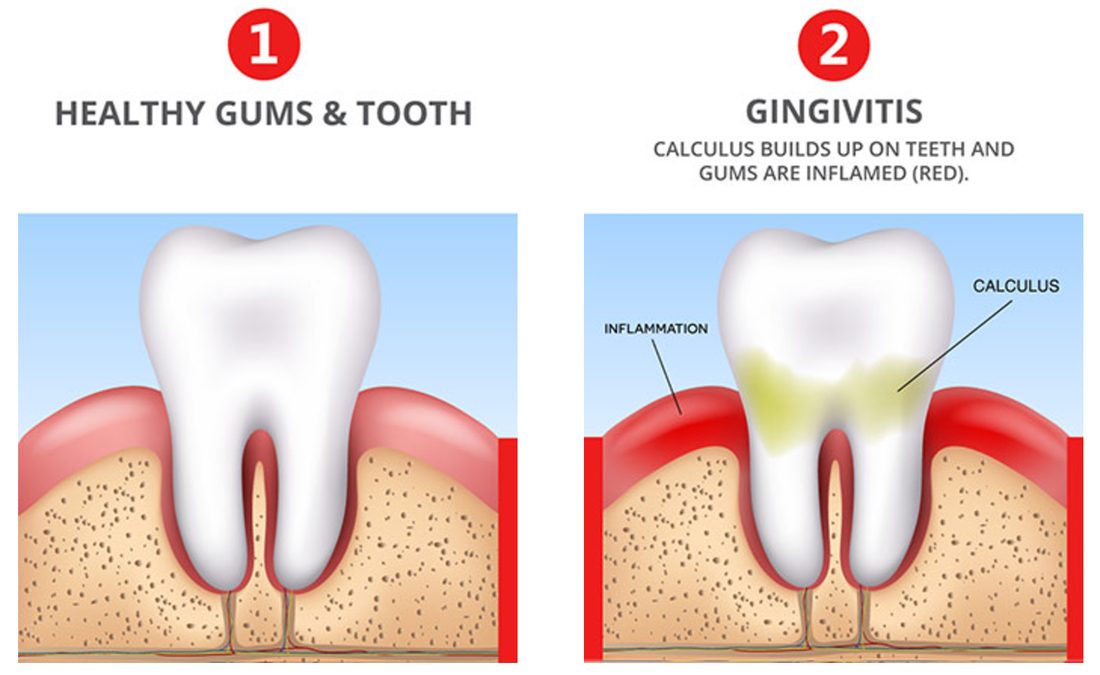
The symptoms of gingivitis include redness and swelling of the gums, tenderness of the gums when touched and bleeding when the teeth are brushed.
Symptom 1: Altered gingival appearance
Changes in appearance are usually described according to colour, shape, size, consistency and surface characteristics. Healthy gingivae are pale pink and the edges of the gum line tightly hug the shape of the tooth. Gingival inflammation usually starts between the teeth and gradually spreads around the tooth margin. The infection causes the tissues to become red and swollen and the fine definition and tone of the gingivae is lost, they eventually become smooth and glossy.
Symptom 2 : Bleeding Gums
Gingival bleeding is probably the most frequent patient complaint. Unfortunately, bleeding is so common that some people may not take it seriously and even believe it to be normal. Bleeding is usually evidence that bacteria are present and an infection has begun. It occurs most frequently while brushing the teeth. Bleeding may also be provoked on eating certain hard foods such as apples. Patients can taste blood and it may even be smelt on the patient’s breath.
Symptom 3: Halitosis – Bad breath and an unpleasant taste
Halitosis describes bad breath, and it often accompanies gingival disease. Halitosis is a common reason why people visit the dentist. The smell originates from blood and poor oral hygiene, and should be distinguished from odours from other sources.
| Stage | Time | Clinical Findings |
| Initial lesion | 2–4 days | Increased gingival fluid flow |
| Early lesion | 4–7 days | Erythema, bleeding on probing |
| Established lesion | 14–21 days | Changes in colour, size, and texture etc |
Risk Factors for Gingivitis
- smoking or chewing tobacco
- diabetes
- certain medications (contraceptives, steroids, anticonvulsants)
- crooked teeth
- dental appliances that fit poorly
- broken fillings
- pregnancy

How Is Gingivitis Treated?
To treat gingivitis you must practice proper oral hygiene. You should also cut back on any smoking and control your diabetes. Other treatments include deep cleaning your teeth, medications, and surgery.
Cleaning Teeth
There are several techniques that can be used to deep clean your teeth without surgery.
- Scaling removes tartar from above and below the gum line.
- Root planning smoothes rough spots and removes infected tooth parts.
- Lasers may cause less pain and bleeding than scaling and root planing.
Medications
- Antimacrobial mouthwash containing chlorhexidine can be used to disinfect the mouth.
- Time-release antiseptic chips containing chlorhexidine can be used after root planing.
- Antibiotic microspheres made with minocycline can be used after scaling and planing.
- Oral antibiotics can be used to treat persistent areas of gum inflammation.
Bleeding Gums / Gingivitis can be prevented by proper and consistent oral hygiene. Make certain to eat a balanced diet and visit the dentist regularly. Brush your teeth twice daily with fluoride toothpaste. Floss your teeth every day.