Endodontics
Root Canal Treatment: Preserving the Tooth
Endodontics is the specialized field of dentistry that deals with the diagnosis, management, and treatment of the infected dental pulp/nerve of the teeth, the surrounding gums, and bony tissue. It is commonly known as root canal treatment.
Endodontics is needed when you have a toothache, i.e. there is pain associated with your teeth, a condition is known as acute pulpitis. This arises when the pulpal tissue/nerves of the teeth are inflamed due to a variety of factors like decay, trauma, large and deep fillings or insults to the tooth.
Root canal treatment is about saving teeth, rather than removing them. In the past, the only way to treat teeth with the disease was to extract them. Now, thanks to modern dental techniques, we are able to save damaged teeth more than 90% of the time. According to your dedicated dentists in Preston; signs to look for diseased pulp; include pain, prolonged sensitivity to heat or cold, tenderness to touch and chewing, discolouration of the tooth, and swelling, tenderness in the lymph nodes as well as nearby bone and gingival tissues. Sometimes, however, there are no symptoms.

How Do We save your Tooth through Endodontics Treatment ?
Thousands of teeth are taken out each year as a result of infection. When a tooth is infected, root canal treatment should be the first choice but instead, patients choose to replace an extracted tooth with a bridge, a dental implant or live with a gap.
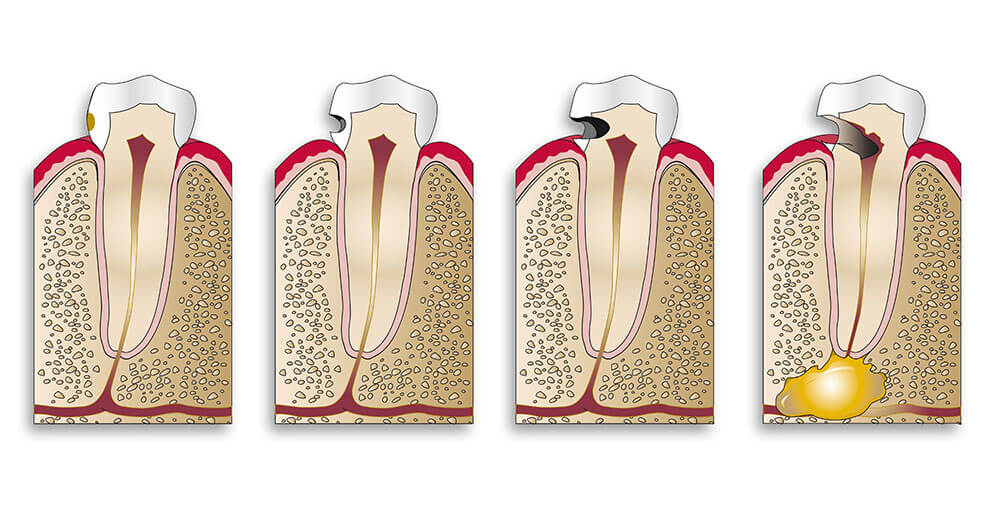
Each tooth has its own nervous and vascular system known as pulp. For a variety of reasons, the pulp of a tooth may become infected with bacteria usually as a result of tooth decay or injury. Because the pulp is in a confined space its ability to overcome infection is quite limited and it is destroyed. Eventually, an abscess forms in the pulp canal and spreads to the adjacent tissues resulting in pain and swelling.
Symptoms of the infection can be identified as visible injury or swelling of the tooth, sensitivity to temperature or pain in the tooth and gums. If you experience any of these symptoms, we will your dentist will most likely recommend non-surgical treatment to eliminate the diseased pulp.
This injured pulp is removed and the root canal system is thoroughly cleaned and sealed. This therapy usually involves local anesthesia and may be completed in one or more visits depending on the treatment required. Success for this type of treatment occurs in about 90% of cases. If your tooth is not amenable to endodontic treatment or the chance of success is unfavorable, you will be informed at the time of consultation or when a complication becomes evident during or after treatment. We use local anesthesia to eliminate discomfort. You will be able to drive home after your treatment, and you probably will be comfortable returning to your normal routine.
What's the Difference between a Dentist and an Endodontist?
While all endodontists are dentists, less than three percent of dentists are endodontists. Just like a doctor in any other field, endodontists are specialists because they’ve completed an additional two or more years of training beyond dental school. Their additional training focuses on diagnosing tooth pain and performing root canal treatment and other procedures relating to the interior of the tooth. In many cases, a diseased tooth can be saved with endodontic treatment. For this reason, endodontists proudly refer to themselves as Specialists in Saving Teeth.
Endodontists Have Advanced Education
To become specialists, endodontists have two to three years of additional education in an advanced specialty program in endodontics after completing four years of dental school. They focus on studying diseases of the dental pulp and how to treat them.
Endodontists Have Specialized Expertise
By limiting their practice to endodontics, endodontists focus exclusively on treatments of the dental pulp. They complete an average of 25 root canal treatments a week, while general dentists typically do two. Endodontists don't place fillings or clean teeth — they dedicate their time to diagnosing and treating tooth pain. They are skilled specialists in finding the cause of oral and facial pain that has been difficult to diagnose.
Endodontists Are Experts in Pain Management
Endodontists use specialized techniques to ensure patients are thoroughly comfortable during their treatments. They are experts in administering numbing medications, especially in patients who traditionally have problems getting and staying numb. In addition to treating you comfortably, patients will be relieved of tooth pain after their treatment when the pulp infection or inflammation heals.
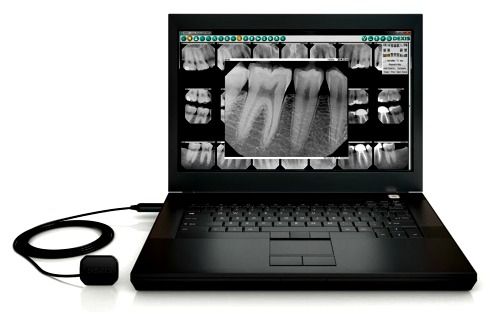
Endodontists Use Cutting-Edge Technologies
Endodontists have materials and equipment designed to make your treatment more comfortable and successful. They use a small sheet of latex called a dental dam to isolate the tooth during treatment, protecting the rest of your mouth. Digital radiographs and 3-D imaging allow endodontists to take detailed pictures of tiny tooth anatomy to better see the root canals and any related infections. Endodontists use dental operating microscopes to better see inside the root canals to thoroughly treat them.

Endodontics as a specialty
If you've reached a point where your dentist says that one of your teeth needs a root canal treatment, how do you decide whether to let him or she carry out the work or have it done by a specialist?
Endodontics was recognised as a dental specialty in the UK only in 1998. In other countries such as the USA and Sweden, this field has been established for many years. Specialty training in Endodontics (Root Canal Treatment) requires three years of formal postgraduate education and goes far beyond the basic endodontics training given to general dentists.
A question of expertise
Some dentists refuse to do any root canals, recognising that the specialist will do a better job. Others will do only the easier cases and there are those that will ‘have a go’ at anything and either refer when they experience difficulties or tell the patient that extraction would be the better option. There are also general practitioners who have developed greater skills in this area. It all comes down to personal experience and expertise.
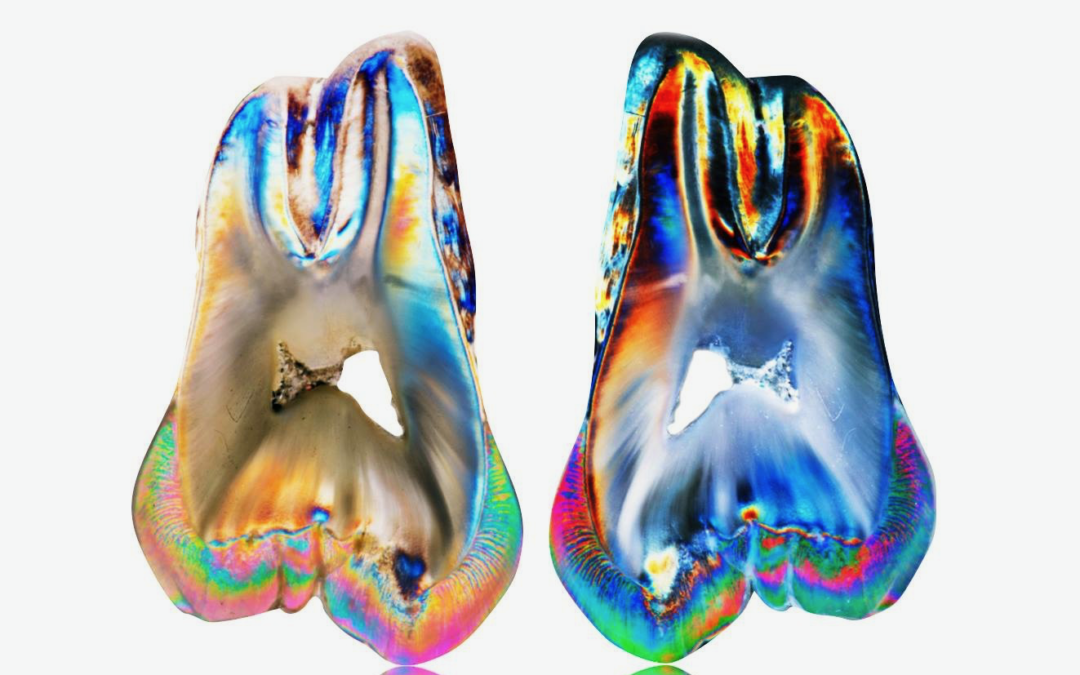
The complexity of dental roots
Some teeth have complex anatomy and generally molar or back teeth have more root canals than front teeth. But in some cases, a molar is easier to treat than a front tooth. Assessing the case is not always easy. One cannot always be guided by a pre-treatment x-ray. It may show that the tooth has curved roots or very small canals that will be difficult to locate. It may look an easy procedure but prove to be challenging in practice, even for a specialist.
Are endodontists more successful?
Generally, yes. The chances of success are very high under the best circumstances, over 95%, but there are no guarantees. Each case must be judged on its own merits. Evidence-based studies suggest that endodontists achieve greater successes due to their experience, expertise, and equipment. Specialists use operating microscopes that give very high magnification and therefore allow work to be carried out with a very high degree of accuracy.
What is Microscope-Assisted Endodontics?
When a tooth becomes severely decayed or damaged, it creates openings for bacteria to grow on the inner parts of the tooth. If the nerves or blood vessels inside the tooth become damaged by the bacteria, the tooth will become painful. If you begin to experience this pain, we can perform a root canal (endodontic treatment) and attempt to save the tooth. Micro-endodontics involves using a microscope, which allows us to see more detail than we would be able to with the naked eye. A few of the key reasons for choosing microscope-assisted endodontics include:
- Improved Accuracy – The dentist will be able to be to make cleaner and more accurate incisions by using smaller instruments during the procedure.
- Minimized incisions – With increased accuracy during the procedure, the surrounding soft tissues in the mouth are less likely to be affected. This will allow for faster healing times and reduce the chances of needing secondary procedures.
- Easier Access – By using the microscope, dentists are able to access areas that are more challenging to reach. Better visualization of the infected area prevents complications.
- Spotting a Fourth Canal – During a traditional root canal, the dentist could easily miss the fourth canal that some teeth have. If this happens, the infection can continue to spread into the bone. By using a microscope, the dentist can spot any hidden canals and clear the infection completely to save the tooth.

Dr Nicole Fender - Specialist Endodontist
General Dental Council No. 68536 ; Qualifying from Cardiff University in 1993 as a qualified Bachelor of Dental Surgery (Dental Surgeon), Dr Fender worked in the hospital service initially, working in general practice whilst completing a Masters Degree in Endodontics in 1998 at Manchester University.
Since 1998 Dr Fender has dedicated her practice to the field of Endodontology (also known as root fillings or root canal treatment) and in 2001 she was recognised by the General Dental Council as a specialist in .Endodontics. Dr Fender recently joined Lane Ends Dental Practice . She treats patients requiring endodontic treatment using an operating microscope and other specialist equipment. She accepts referrals for this treatment from colleagues within the practice, and from many other Dental Practices across the region.
Dr Fender is also a part-time tutor at Manchester Dental Hospital where she is involved in the clinical teaching of Endodontics to post-graduate students. Dr Fender is registered with the General Dental Council and a member of the British Endodontic Society.She is also the Secretary for the North-West Endodontic Study Circle (Norwesc), a group of Specialist Endodontists based in the North West. Dr Fender attends conferences and courses on a regular basis to ensure she is fully up to date with new developments. Dr Fender offers payment plans, and uses up to date protocols of treatment at the competitive prices and welcomes new referrals.
The referral process
Referred patients will only be accepted for the specific treatment requested by the referring dentist. After an initial consultation, options and choices available to the patient will be discussed in detail and Dr Fender will spend as much time as necessary to enable patients to make an informed decision about the appropriate treatment for their needs.
A fully personalised treatment plan and estimate of the fees involved will be given to the patient. No treatment will be carried out until this has taken place.
Once Dr Fender has completed the treatment for which the patient has been referred, they are returned to the referring dentist who will complete any ongoing treatment. A full written report will be sent to the referring dentist.
When making the referral, it is appreciated that as much as possible information about the case is passed on to Dr Fender. This can save the patient time and money.
Root Canal Referral Charter;
-
- We will always return the patient to the referring dentist.
-
- We aim to contact patients within 24 hours.
-
- We will return patients' and dentists' calls within 24 hours if they have any queries.
-
- The patient will receive a detailed treatment plan and all costs will be agreed and discussed before treatment.
-
- We will always provide recommendations for further care.
-
- We will only carry out treatment in accordance with instructions from the referring dentist.
-
- No further treatment will be carried out without authorisation from the referring dentist.
-
- We will keep you updated throughout the treatment.
-
- We aim to send a full treatment report to the referring dentist within two working days.
-
- We only use the most modern and scientific proven procedures, materials and equipment.
- We will offer reasonable and highly competitive specialist fees.

Is Root Canal Treatment Painful
The perception of endodontic therapy being painful began decades ago when root canal treatment methods were quite primitive and painful. But with the latest technologies and anaesthetics, root canal treatment today is no more uncomfortable than having a filling placed. In fact, a recent survey showed that patients who have experienced root canal treatment are six times more likely to describe it as “painless” than patients who leave their infected teeth untreated.
Local anaesthesia is used and we also take every measure to ensure that your procedure is in no way uncomfortable or painful. For most patients, the feeling of numbness usually subsides after 2-3 hours.It is normal for teeth to be sore for a few days after root canal treatment. Some teeth, particularly ones that have been problematic for a while, may take a few months to settle. This discomfort is normally from the inflamed supporting tissues.
DO I need to see my dentist after a Root Canal Treatment ?
If you have been referred to us, when your root canal therapy has been completed, a record of your treatment will be sent to the dentist who referred you. We advise you to return to your general dentist between two to four weeks after your root canal treatment is completed to have your final restoration done unless advised differently by us. This amount of time will allow most of your tenderness to subside before having further procedures done on your tooth. If your tooth does not get the necessary final restoration (crown or filling) and the temporary filling wears out, the root canal will become infected and need retreatment.
The final restoration is either a filling or a crown and will be placed to protect your tooth from fracture and further contamination and restore your tooth to its full function. As the unrestored tooth is susceptible to fracture, please do not chew or bite on the treated tooth until you have it restored by your dentist.
Final Verdict: Root Canals Are Preferred, but Not Always Possible
Between a root canal and a tooth extraction, a root canal is often the preferred choice because it works on fixing your natural tooth so that it could remain in place. However, a root canal may not always be an option, depending upon the damage that a tooth has incurred. If a tooth is far too compromised, your dentist might recommend an extraction, followed by a dental implant to replace what was lost.
